Payers are transforming processes, technology, and teams to better attract, retain, and engage consumers, yet siloed data and disparate point solutions continue to challenge momentum. Our thought leaders in CRM and digital health, Michael Porter and David Allen, recently addressed these challenges in a session titled “Improve Outcomes, Drive Growth, Boost Experiences: Pragmatic, Revolutionary CRM” at the AHIP Consumer Experience & Digital Health Forum. In their talk, Michael and David discuss ways payers can deploy customer relationship management (CRM) technology to:
- Personalize outreach
- Enhance customer service
- Elevate care and disease management
- Optimize utilization management
Here are five key takeaways from the session:
1. Healthcare consumers desire a seamless journey
Consumers do not want experiences that fragment as they move between patient and member environments and between periods of care. Seamlessness requires breaking down silos. We see silos and legacy systems in almost every payer we work with, and executives are frustrated. Using CRM as an integrated center of experiences is a key part of getting past silos and creating a more seamless journey. CRM plays a role in allowing you to communicate with consumers based on where they are in the lifecycle, for more integrated and relevant messages. A better, more seamless, customer experience yields increased conversion rates, higher satisfaction, and ultimately, better health outcomes.
READ NOW: Healthcare CRM: Evolving Beyond Your Legacy Platform
2. CRM delivers more than marketing automation
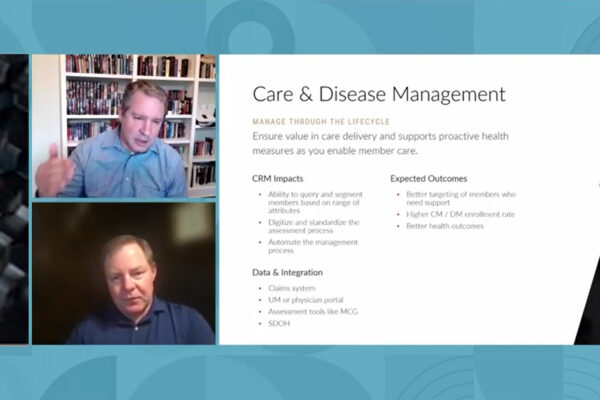
CRM in the payer space can very quickly expand well beyond traditional marketing use cases, contact management, and basic relationship management. It can also include a 360-degree view of your stakeholders and business health, automated processes, actionable insights and much more to create a better end-to-end experience. For payers, the platform also offers useful outcomes for broker management, sales, enrollment, network management, call center, care and disease management, and utilization management. There are many applications to make consumer experiences richer.
LEARN MORE: More CRM Use Cases for Payers and Providers
3. CRM allows for continuous improvement
CRM allows you to draw inferences and use those inferences to make continuous improvements. This platform enables you to use CRM as a decision engine and a source of intelligent automation. Through AI and machine learning, decision making is built into your organization. This is not only applicable for a wide range of use cases. It also means that you can turn your data into reliable, actionable understanding to act quickly and continuously.
4. Payers can create HIPAA compliant communications
Many payers don’t think they need marketing automation because they are not allowed to talk to their members, especially using claims data. Regulations must be carefully followed, and consumers care about transparency with how their data is being used. However, there are still many things you can do with data for effective, HIPAA compliant, and respectful targeted communications. This can be done for core use cases, wellness improvements, plan journey tracking, Medicare conversions, and more. There is no reason payers can’t both comply and use CRM to create a personalized journey and set that journey on its path.
READ MORE: How to Create a Better Consumer Experience While Still Taking HIPAA Into Account
5. CRM is not an end-all-be-all
CRM attempts to make processes better. However, it is not the end-all-be-all solution. Simply implementing a system is not the end of the process. You must continuously use the insights delivered to make improvements. CRM is the glue that ties things together. If this glue is utilized correctly, you will see both higher productivity and lower costs.
EXPLORE NOW: How Perficient Crafts the Best CRM Approach for Your Business
Want to learn more about how CRM can help payers better attract, retain, and engage consumers? We invite you to learn more by watching the full recording of our AHIP session below.
Our digital healthcare experts are here to help. Contact us to discuss your specific goals.