Healthcare payers and provider groups across the country are challenged with high costs and long provider onboarding durations due to a lack of integrated automated processes. Organizations often rely on multiple systems and manual processes to onboard and manage providers, resulting in high Center for Medicare & Medicaid Services (CMS) fines due to poor data management.
Our Provider Onboarding and Administration (POA) solution is a digital solution that can be used by payers to efficiently manage provider enrollment and the credentialing process. Built on Pega’s Healthcare Foundation Data Model, Perficient’s solution leverages Pega’s low-code platform and case management to achieve operational efficiency and improve customer satisfaction.
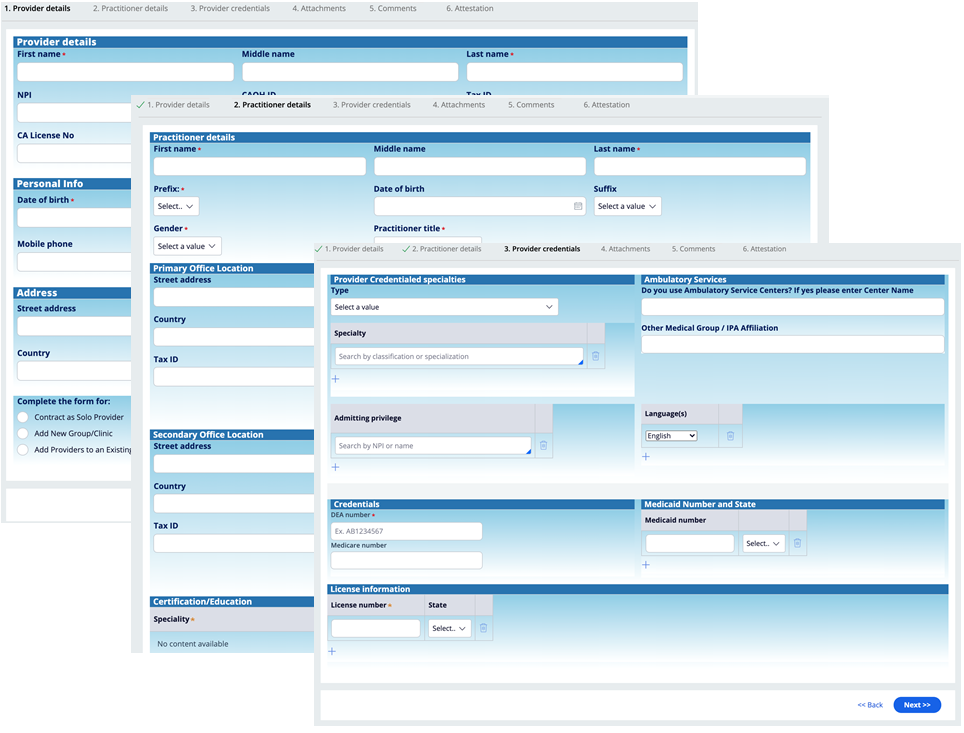
POA provides end-to-end provider data management that begins with the provider online application via a self-service portal and goes through credential validation, contracting, and ongoing management.
Watch our Pega POA video for key highlights:
https://youtube.com/watch?v=g9T78kaai70%3Frel%3D0
Key Features
- Leverages Pega’s low-code platform and case management to achieve operational efficiency and improve customer satisfaction
- Provides end-to-end provider data management
- Integrated provider source verification during credentialing process increases throughput and reduces manual effort
- Continually tracks deadlines and renewal requirements for various licenses, certificates, continuing medical education, and other medical requirements
- Shortens the time to onboard providers, resulting in greater provider satisfaction and reduced CMS fines
Benefits
- Provider enrollment and credentialing for commercial insurance, Medicare, and Medicaid
- Medicare and Medicaid revalidation form generation to maintain billing privileges (PECOS)
- CAQH integration
- NPI registrations (Type I and Type II)
- Managed care contracting
- Hospital privileging
- Real-time application status dashboard
- Supplement/source of truth for Find-a-Doc
- Breaking down siloed systems for single view without custom development
- Automate manual ad hoc processes
- Paperless contracting and records
- Improved provider satisfaction and significant reduction in onboarding time from 6-18 months to 6-8 weeks
- Save 1-3x salary costs by retaining providers
The Provider Journey
- The provider will apply through a self-service portal
- Credentialing will validate license, certifications, and specialties using Primary Source Verifications for providers
- Contracts are then auto generated based on provider type
- Provider details are then loaded into internal systems, triggering a welcome letter email and granting the provider access to the provider portal
- Provider requirements are continually tracked and the provider receives notification’s for deadline and renewal requirements.
Self-Service Portal
Our self-service process gathers the pertinent provider data (e.g., personal, demographic, specializations, certifications) and any necessary documents. This stage is where we benefit greatly from rapid UI prototyping enabled by the Pega platform’s app and dev studio. Onboarding flow can also be embedded as mashup in an existing external customer portal.
Credentialing
Solution has pre-built integrations to verify provider credentials, including:
- Validate NPI (https://npiregistry.cms.hhs.gov)
- State provider verification (https://data.wa.gov)
- USPS address verification
- National Practitioner Data Bank (https://www.npdb.hrsa.gov/)
These processes are performed in parallel to reduce processing time. Portal dashboard provides real time status, and email and text notifications can be configured to give regular updates.
Contracting and Onboarding
The contracting process generates the contract documents specific to the provider type once committee approval is granted. Providers have the ability to review and approve contracts via the application. Contracts are delivered to provider via DocuSign for e-signature.
The onboarding process generates the onboarding letter and delivers it via email. Provider data is persisted in back end systems and secure access to provider portal is granted. Provider portal credentials are delivered via email.
Ongoing Management
Pega’s built-in analytical tools give ongoing tracking that we use for dashboard status, auditing, and reporting. Particularly, they enable tracking of certification and licensing deadlines as well as renewal tasks.
Perficient and Pega
As a Pega Alliance Partner and Pega Partner Advisory Council Member, we are experienced in identifying and solving the unique challenges of our clients with award-winning cloud and BPM solutions. We partner with Pega to provide industry-leading case management, BPM, CRM, and robotics solutions that eliminate inconsistent user experiences and overly complicated systems. Learn more about our partnership here.

