As a registered nurse (RN), I’m in the field of medical and nursing terminologies within electronic health records (EHRs). I understand all too well the impact and benefits that standard healthcare terms contribute to leveraging interoperability and providing healthcare with big data for research and population health, and why it’s a lot easier said than done.
The Difficulties of Standardizing Healthcare Terms
Physicians, nurses, and other healthcare professionals face numerous challenges when documenting their assessments and diagnoses with associated labs, tests, and procedures located within an EHR from standardized coding systems, such as ICD-9, ICD-10, CPT, LOINC, etc. We are forced to sometimes associate tests and procedures with diagnoses or conditions that aren’t exactly what the patient presents with. A good example of this is when a patient presented with lower abdominal pain and upon further exam and diagnostic CT, the patient was found to have a somewhat rare condition called epiploic appendagitis. When the physician was forced to pick from a list of ICD-9 codes to associate the CT scan he ordered, there was no option for epiploic appendagitis. So he went with the next best option, diverticulitis. These two conditions are not one in the same and showcases some of the obstacles healthcare providers face when having to pick from a list of standardized terminologies within an EHR.
The frustration lies in the multitude of ways that having to describe a condition made available from a standardized list of coded diagnoses and assessments causes complexities. This is a common pain point for many healthcare providers who feel that standardization doesn’t capture the true essence of a patient or care provided. These providers continue to document their findings and diagnoses as unstructured data in EHRs through dictation and narratives. This makes it extremely difficult to map or extract data for research, billing purposes, etc.
Another impediment that some physicians express, is the amount of effort that they put towards trying to find the right diagnosis from a list of standardized terminologies, as this takes away valuable face time with patients. The challenge behind standardization is mainly due to the fact that the medical field is vastly complex and ever changing. It is nearly impossible to come up with one standardized list of terminologies across the board that satisfy everyone’s needs. Also, due to the variation of vocabularies found within different EHRs, mapping presents a major hurdle to interoperability. It also begs the question of how to continually update the standardized lists as new terminologies are created and old ones are retired? But without standardization, how do we overcome the uphill battle of interoperability and communication between a myriad of EHRs and terminologies?
SUCCESS IN ACTION: Empowering Healthcare Consumers and Their Care Ecosystems With Interoperable Data
The Benefits of Standardizing Healthcare Terms
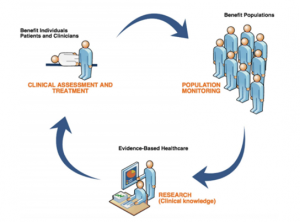
The advantages of standardizing healthcare terms outweigh the major efforts required to combat the issue around unstructured data and interoperability. There are several national initiatives that share the goal of standardizing vocabularies within EHRs to facilitate the transfer of data, information, and knowledge among systems with the ultimate goal of interoperability. Meaningful use is one of the main drivers for interoperability with a foundation based upon priorities to improve quality, safety, efficiency, population and public health, and reducing health disparities. Finding a way to overcome the variability in which clinical data is portrayed, is extremely important in interoperability and big data. We have all this clinical data within EHRs, databases, and data warehouses that can be used for research and population health, but we are unable to easily extrapolate this data due to the lack of standardized terminologies and unstructured data.
READ MORE: How Our Data Integration and Other Capabilities Are Helping Reduce Health Disparities
What about Standardizing Nursing Terminologies?
Most people have heard of interoperability and the need to standardize healthcare terms, but what about nursing terminology? Nurses provide more direct patient care than physicians, and therefore provide extensive ongoing documentation regarding assessment, treatment, and outcomes of patient care. I’m somewhat partial to this subject and to the fact that you mostly only hear about standardized medical terminology.
Documented nursing care tends to fall under the radar when it comes to hospital and accounting information systems and EHRs. One of the major contributors to this phenomenon is the lack of structured nursing data to represent the care that nurses provide. It’s just as important to continue to support and produce a scientific classification of nursing work as it is in medicine.
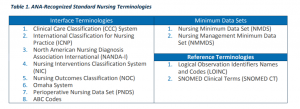
Standardized nursing data has the ability to provide decision support, discovery of disparities, reporting of outcomes, improved performance, maintenance of accurate problems lists and medications, and the ongoing exchange of information and data as referenced by the Alliance of Nursing Informatics (Sensmeier, 2010, p.66). The American Nurses Association (ANA) recognizes 12 standardized nursing terminologies. The Omaha System is just one system that creates standardized data that can then be used for “meaningful use applications such as exchange of patient and population information, healthcare quality evaluation, and health services research” (Martin, Monsen, & Bowles, 2011). Another great example is the International Classification for Nursing Practice (ICNP), which provides a structured vocabulary, classification, and a framework into which existing terminologies and classifications can be cross-mapped to allow comparison of nursing data.
READ NOW: Who is Filling the Gap in the Clinical Terminology World?
The Future of Standardized Healthcare Terms and Interoperability
It’s not just medicine that faces this daunting challenge of finding a way to create interoperability through standardized healthcare terms. All realms of patient care, including nursing are affected since interoperability is reliant on medicine and nursing working together to overcome this national and global obstacle.
The Systematized Nomenclature of Medicine – Clinical Terms (SNOMED CT) holds promise as it is one of the most comprehensive, multilingual clinical healthcare terminologies that is reliable in representing clinical data in EHRs, and it maps to other international standards. SNOMED CT offers more unique concepts across a wider range of multidisciplinary clinical data than other terminologies and is able to provide mapping to ICD-9 and ICD-10 codes. It is also required in the Office of the National Coordinator (ONC) Health IT Certification Program, which is a voluntary certification program established by the Office of the National Coordinator for Health IT.
The International Health Terminology Standards Development Organization (IHTSDO), which owns and maintains SNOMED CT is continuing to work with the International Council of Nurses (ICN) in developing and maintaining an equivalence table of nursing diagnoses and interventions between SNOMED CT and the ICNP. There is also an IHTSDO Nursing Special Interest Group that supports the development and implementation of SNOMED CT in ensuring it supports nursing requirements for electronic documentation in the EHR (https://www.healthcareitnews.com/news/icn-and-ihtsdo-collaborate-improve-care-through-standardization).
The future of standardization and interoperability is looking brighter, with ongoing national initiatives and continued development and partnership of standard healthcare terminologies, such as SNOMED CT and ICNP in both medicine and nursing.
LEARN MORE: Barriers to Healthcare Data Standardization
Partner With Perficient
Healthcare and Life Sciences leaders rely on us for strategic and technical expertise to achieve their missions in a technologically advancing industry. We are uniquely qualified to meet your standardization and interoperability needs. The 10 largest health systems and 10 largest health insurers in the U.S. have counted on us to support their end-to-end digital success. Modern Healthcare has also recognized us as the fourth largest healthcare IT consulting firm.
Our thought leaders are here to support you in achieving business goals and solving your most complex technology challenges with pragmatic, strategically-grounded know-how. With more than 20 years of experience in the healthcare industry, Perficient is a trusted, end-to-end, global digital consultancy. Contact us to learn more.
References
Martin, K.S., Monsen, K.A., Bowles, K.H. (2011). The Omaha System and Meaningful Use: Applications for Practice, Education, and Research. CIN: Computers, Informatics, Nursing, 29 (1), 52-58. https://www.ncbi.nlm.nih.gov/pubmed/21099545
Sensmeier J. Alliance for Nursing Informatics statement to the Robert Wood Johnson Foundation Initiative on the Future of Nursing: acute care focusing on the area of technology. Comp Inform Nurs. 2010;28(1):63–67. https://www.ncbi.nlm.nih.gov/pubmed/19940623
The Office of the National Coordinator for Health Information Technology. (2017). Standard Nursing Terminologies: A Landscape Analysis. https://www.healthit.gov/sites/default/files/snt_final_05302017.pdf
Editor’s Note: This post was originally published in July 2019 and has been revamped and updated for accuracy and comprehensiveness.