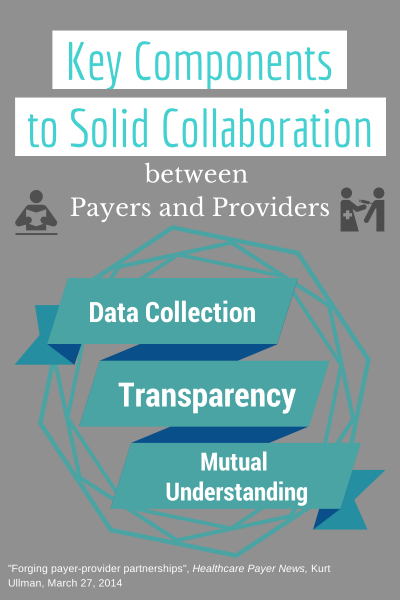
There is no doubt that the relationship between payers and providers is beginning to change, evolving from challenging and adversarial interactions into more collaborative exchanges. Kurt Allman, in his article in Healthcare Payer News this week, outlines 3 components for this relationship to be successful:
- Data collection
“Payers collect a lot of data, which can provide a broad picture of what is happening in a population and across the entire continuum of care. Health systems bring a rich vein of information related to specific components of that continuum.” - Transparency
“We rely on this data to make sure we know what works, and when it doesn’t work, we use the information to identify opportunities for improvement,” says Kevin Sears, vice president of payer strategy and product development at CHE Trinity Health in Lavonia, Mich. - Mutual understanding
In the past, providers worked to drive up revenue from the payer, while the payers needed to drive down costs to please their customers, both employers and employees/members. Now the two have to work together to reduce waist and improve care.
Now, we see that payers and providers must collaborate in order to truly drive value, more so than they ever needed to in the past.
When payers and providers work together to achieve all three of the above imperatives, they’ll identify opportunities that will become mutually beneficial. Each can begin by asking themselves whether their high-priority projects are working to help them to obtain higher transparency, data collection and sharing, and a mutual, more collaborative relationship with the other.