We are at the AHIP Conference this week, which is one of our favorite events of the year. It is good fun to meet with the many tech-savvy professionals that make up the health insurance industry. This year we meet as many regulatory pressures and deadlines are closing in, which is certain to ignite some excellent conversations and knowledge sharing.
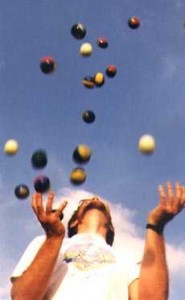
Leaders in the healthcare industry are juggling a series of regulatory deadlines and are struggling to keep up. With 5010, ICD-10, ACO, HIPAA privacy updates, and Meaningful Use, many feel that there are just too many IT projects to keep straight. With regard to ICD-10, and the prerequisite 5010 transaction set, survey after survey has shown that the healthcare industry is procrastinating. This is not a surprise. Fair or not, the healthcare industry has a reputation for procrastination. One main reason for this procrastination is the hope that the government will blink and push back deadlines. This game of chicken could prove very costly.
On the provider side, if organizations do not meet the October 1, 2013 deadline, then they will not be able to bill health plans for services. These deadlines can represent a tremendous cost burden as a result. If things continue at this rate, then health plans may start receiving claims in both ICD-9 and ICD-10. Imagine the administrative burden of running two operating systems at the same time. If they choose not to take on the burden of a dual system, these health plans will need to decide if a claim transmitted with the old ICD-9 code set will be rejected. Doing work and not getting paid for it is the ultimate cost of procrastination. Even a 1% decrease in revenues could prove disastrous.
Reward for the Pain of 5010 and ICD-10
Many feel that there are just too many IT projects on the table at once. However, the transition to ICD-10, and the 5010 precursor, are not just IT projects. These changes denote a transformation in the way of doing business in healthcare. This is particularly true for health insurance plans. This is because data integration is key to completing these conversions. There are numerous siloed data systems across a healthcare organization in terms of clinical systems, claims, A/R, etc. which become integrated as a result of remediation. This data integration in and of itself creates a bevy of “next generation” operational benefits, such as those experienced by BCBS of Massachusetts. As highlighted in an earlier post, there is a reward for the pain of 5010 and ICD-10. These rewards include:
- A new level of transactional analysis by virtue of the expansion of the sheer number of new codes from ICD-9
- The ability to generate more specific clinical data for quality metrics and tracking of resource use, which could save money
- Improving the quality of operations and the level of understanding in a complex healthcare business, which can save time, money and maximize return in the long run for the U.S. healthcare delivery system
- The ability to re-structure how a healthcare organization views its service lines for operations and profitability
- Analysis, database remediation, database migration and testing brings a new detailed capability to examine the profitability and costs by procedure, the costs of specific diagnoses, and potential operational savings from best practice
- Using re-worked analytic reports built around ICD-9 codes to examine the bigger picture of how business intelligence, decision support and analytics should perform
- New opportunities for building more comprehensive data marts and stronger operational reporting including digital operations dashboards
- For the more progressive IT teams, ICD-10 remediation could be an opportunity to move to a self-service model for reporting that capitalizes on a new generation of business intelligence tools
The best advice to healthcare organizations watching the ICD-10 time clock: Don’t treat ICD-10 as just another compliance issue. Instead, use this as an opportunity to transform into a world-class healthcare organization.