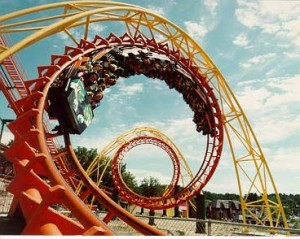
 Opinions and posturing on the Accountable Care model started well before the release of the proposed regs over a month ago. However, since their release those of us working within the healthcare industry have been riding the rollercoaster of public sentiment. The enthusiasm around the regs was immediate upon their release. Blogs, Twitter, and online news sources were filled with ACO stories. It was difficult to find news on any other subject in those first few days. Unlike some of the other trends we follow in healthcare, ACO stories even began to filter out into the mainstream.
Opinions and posturing on the Accountable Care model started well before the release of the proposed regs over a month ago. However, since their release those of us working within the healthcare industry have been riding the rollercoaster of public sentiment. The enthusiasm around the regs was immediate upon their release. Blogs, Twitter, and online news sources were filled with ACO stories. It was difficult to find news on any other subject in those first few days. Unlike some of the other trends we follow in healthcare, ACO stories even began to filter out into the mainstream.
Negative sentiment around the regs came in waves and hit a crescendo last week with news that the American Medical Group Association, and the 400 medical groups they represent, are not fans of the proposed regs. One chief objection is the investment required to become an ACO. This was quickly followed today with the administration offering a new path toward Accountable Care.
Like David Harlow of HealthBlawg, many believe that “reasonable minds can improve the draft regulations”. After all, this is the purpose of putting the regs out for comment in the first place, no? I personally feel that regardless of the way in which the model is ultimately referenced, ACO or otherwise, many of the elemental components of Accountable Care will live on regardless. This is particularly true when it comes to the Health IT components that underpin the Accountable Care model. These include:
- Increased Data Exchange in Health Communities: Fragmented data across healthcare communities leads to increased cost and decreased patient experience. The ability to exchange clinical information is critical to Accountable Care success, but is gaining steam independent of the ACO movement as well. Beyond the important aspects of delivering quality care, there are real business drivers that favor an environment where clinical and cost information are combined into a comprehensive system delivery model. The Enterprise HIE eco-system is one approach that innovative healthcare systems are using to enable them to connect patients and physicians together in a more collaborative environment.
- Increased Collaboration Among Patients, Physicians, and Healthcare Communities: Enabling patients and physicians into the design of care increases the financial effectiveness under the Accountable Care model, but movement around healthcare consumerism and patient-centered medical homes are driving toward the same end. Healthcare portals can be used to empower patients by providing meaningful access to their care and connect a patient to the entire health system that impacts their care. Similarly, community portals are being created to connect patients to those with similar disease states for information sharing, support, and advice. This empowers patients to work with their healthcare providers in creating cost saving, and patient centric, clinical care. Organizations are also using physician portals to connect physicians to the critical components of clinical care which are then incorporated into executive decision making. This would enable stakeholders of a healthcare system to come together to create better services and relationships within the community that they serve and increase Accountable Care success as well.
So, what do you think is around the next bend for the Accountable Care model?
