On April 11, 2016, the Centers for Medicare and Medicare (CMS) announced an initiative called the Comprehensive Primary Care (CPC+). This initiative, which builds on CMS’s previous Comprehensive Primary Care (CPC) initiative, is designed to “improve the quality of care patients receive, improve patients’ health, and spend health care dollars more wisely 1” and similar to the CPC initiative will focus on the five key comprehensive primary care functions: (1) Access and Continuity; (2) Care Management; (3) Comprehensiveness and Coordination; (4) Patient and Caregiver Engagement; and (5) Planned Care and Population Health.
CMS describes CPC+ as “a national advanced primary care medical home model that aims to strengthen primary care through a regionally-based multi-payer payment reform and care delivery transformation. CPC+ will include two primary care practice tracks with incrementally advanced care delivery requirements and payment options to meet the diverse needs of primary care practices in the United States (U.S.). The multi-payer payment redesign will give practices greater financial resources and flexibility to make appropriate investments to improve the quality and efficiency of care, and reduce unnecessary health care utilization. CPC+ will provide practices with a robust learning system, as well as actionable patient-level cost and utilization data feedback, to guide their decision making 1.”
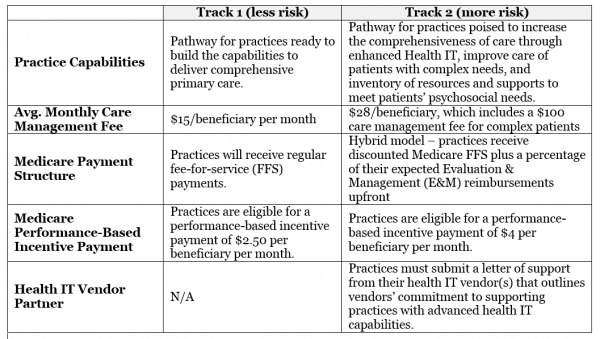
According to VMG Health, CPC+ is expected to involve up to 5,000 practices and 20,000 physicians in 20 regions, amounting to over 25 million patients, throughout its five-year plan starting January 2017 and providers can participate in CPC+ under two tracks, which will both provide a monthly care management fee and upfront performance-based incentive payments, the latter of which is subject to return at year end if certain quality and utilization standards are not met 2. Key difference between the two tracks are as follows:
The Upside
The upside to CPC+ is the goal to shift from the traditional reactive, episodic-driven, fee-for-service model to a more proactive, comprehensive, value-based care delivery model has good intentions. To further support this methodology, CPC+ has identified five key components it’s aiming to achieve, at minimum 3:
- Support patients with serious or chronic illnesses to achieve their optimum health status
- Give patients 24-hour access to care and health information
- Deliver preventive care services to patients
- Engage patients and their families in their own care
- Coordinate the care of patients with other providers in the market
In order to hit the mark on these types of services, healthcare organizations are without a doubt going to have to heavily foster an IT dependent, data centric, collaborative approach amounts all the players. The support for is evident by CMS requesting vendors, within Track 2, to sign a Memorandum of Understanding (MOU) with CMS that outlines their commitment to supporting practices enhancement of health IT capabilities. Increasing the holistic model through information sharing is key to delivering the proactive, information driven, high-value care the initiative looks to accomplish.
In addition, according to analysis conducted by Paul Ginsburg, Margaret Darling, and Kavita Patel of the Brookings Institute, “The combination of larger per beneficiary monthly payments and lower payments for services is the most important part of the initiative. By blending capitation (monthly payments not tied to service volume) and FFS (fee-for-service), this approach might achieve the best of both worlds4.” The analysis also highlights the impact of increasing payments to access to care through maintaining primary care physicians, “An advantage of any program that increases payments to primary care practices is that it can partially compensate for a flaw in the relative value scale behind the Medicare physician fee schedule. This flaw leads to underpayment for primary care services. Higher payments for primary care practices through the CPC+ can help slow the degree to which physicians are leaving primary care until more fundamental fixes are made to the fee schedule.4”
The Potential Downside
As with most things in this world, with the good could come the potential bad. Though the CPC+ program certainly is in the right mind set to drive quality care via a more comprehensive delivery model, the Brookings Institute analysis notes two potential missed opportunities 4:
- The lack of incentives for primary care physicians to take steps to reduce costs for services beyond those delivered by their practices. These include referring their patients to efficient specialists and hospitals, as well as limiting hospital admissions. There are rewards in CPC+ for lower overall utilization by attributed beneficiaries and higher quality, but they are very small.
- The inability of physicians participating in CPC+ to participate in accountable care organizations (ACOs). One of [Centers of Medicare and Medicaid Innovation’s] challenges in pursuing a wide variety of payment innovations is apportioning responsibility across the programs for beneficiaries who are attributed to multiple payment reforms. As a result, ACOs are no longer rewarded for using certain tools to address overall spending, such as steering attributed beneficiaries to efficient providers for an episode of care or encouraging primary care physicians to increase the comprehensiveness of the care they deliver
The critical role primary care plays in reducing overall healthcare cost is well accepted and little to no argument should be made against initiatives that improve various aspects of its delivery whether clinical, operational and/or financial. What seems to be up for debate is, which of countless initiative does an organization/practice participate? Given that there seems to be overlapping and perhaps contradictory initiatives in place, it may be time to take a good hard look at the present state of healthcare and reassess, prioritize and, if needed, decommission those initiatives that are no longer applicable or can be replaces by one more suitable based on a more innovative path to drive optimal quality of care while reducing overall spend on healthcare.
What do you think? Do you think CPC+ will drive changes in primary care practices?
Resources for this blog post:
- https://innovation.cms.gov/initiatives/comprehensive-primary-care-plus
- http://vmghealth.com/comprehensive-primary-care-plus-fair-market-value/
- http://www.mckesson.com/blog/assessing-practice-readiness-for-medicares-comprehensive-primary-care-plus-initiative/
- https://www.brookings.edu/2016/05/31/cmmis-new-comprehensive-primary-care-plus-its-promise-and-missed-opportunities-2/